FEAR ITSELF
Dating back to antiquity, influenza pandemics have posed the greatest threat of a worldwide calamity caused by infectious disease. Over the past 300 years, ten influenza pandemics have occurred among humans. The most recent came in 1957-58 and 1968-69, and although several tens of thousands of Americans died in each one, these were considered mild compared to others. The 1918-19 pandemic was not. According to recent analysis, it killed 50 to 100 million people globally. Today, with a population of 6.5 billion, more than three times that of 1918, even a "mild" pandemic could kill many millions of people.
A number of recent events and factors have significantly heightened concern that a specific near-term pandemic may be imminent. It could be caused by H5N1, the avian influenza strain currently circulating in Asia. At this juncture scientists cannot be certain. Nor can they know exactly when a pandemic will hit, or whether it will rival the experience of 1918-19 or be more muted like 1957-58 and 1968-69. The reality of a coming pandemic, however, cannot be avoided. Only its impact can be lessened. Some important preparatory efforts are under way, but much more needs to be done by institutions at many levels of society.
THE BACKDROP
Of the three types of influenza virus, influenza type A infects and kills the greatest number of people each year and is the only type that causes pandemics. It originates in wild aquatic birds. The virus does not cause illness in these birds, and although it is widely transmitted among them, it does not undergo any significant genetic change.
Direct transmission from the birds to humans has not been demonstrated, but when a virus is transmitted from wild birds to domesticated birds such as chickens, it undergoes changes that allow it to infect humans, pigs, and potentially other mammals. Once in the lung cells of a mammalian host, the virus can "reassort," or mix genes, with human influenza viruses that are also present. This process can lead to an entirely new viral strain, capable of sustained human-to-human transmission. If such a virus has not circulated in humans before, the entire population will be susceptible. If the virus has not circulated in the human population for a number of years, most people will lack residual immunity from previous infection.
Once the novel strain better adapts to humans and is easily transmitted from person to person, it is capable of causing a new pandemic. As the virus passes repeatedly from one human to the next, it eventually becomes less virulent and joins the other influenza viruses that circulate the globe each year. This cycle continues until another new influenza virus emerges from wild birds and the process begins again.
Some pandemics result in much higher rates of infection and death than others. Scientists now understand that this variation is a result of the genetic makeup of each specific virus and the presence of certain virulence factors. That is why the 1918-19 pandemic killed many more people than either the 1957-58 or the 1968-69 pandemic.
A CRITICAL DIFFERENCE
Infectious diseases remain the number one killer of humans worldwide. Currently, more than 39 million people live with HIV, and last year about 2.9 million people died of AIDS, bringing the cumulative total of deaths from AIDS to approximately 25 million. Tuberculosis (TB) and malaria also remain major causes of death. In 2003, about 8.8 million people became infected with TB, and the disease killed more than 2 million. Each year, malaria causes more than 1 million deaths and close to 5 billion episodes of clinical illness. In addition, newly emerging infections, diarrheal and other vector-borne diseases, and agents resistant to antibiotics pose a serious and growing public health concern.
Given so many other significant infectious diseases, why does another influenza pandemic merit unique and urgent attention? First, of the more than 1,500 microbes known to cause disease in humans, influenza continues to be the king in terms of overall mortality. Even in a year when only the garden-variety strains circulate, an estimated 1-1.5 million people worldwide die from influenza infections or related complications. In a pandemic lasting 12 to 36 months, the number of cases and deaths would rise dramatically.
Recent clinical, epidemiological, and laboratory evidence suggests that the impact of a pandemic caused by the current H5N1 strain would be similar to that of the 1918-19 pandemic. More than half of the people killed in that pandemic were 18 to 40 years old and largely healthy. If 1918-19 mortality data are extrapolated to the current U.S. population, 1.7 million people could die, half of them between the ages of 18 and 40. Globally, those same estimates yield 180-360 million deaths, more than five times the cumulative number of documented AIDS deaths. In 1918-19, most deaths were caused by a virus-induced response of the victim's immune system—a cytokine storm—which led to acute respiratory distress syndrome (ARDS). In other words, in the process of fighting the disease, a person's immune system severely damaged the lungs, resulting in death. Victims of H5N1 have also suffered from cytokine storms, and the world is not much better prepared to treat millions of cases of ARDS today than it was 85 years ago. In the 1957-58 and 1968-69 pandemics, the primary cause of death was secondary bacterial pneumonias that infected lungs weakened by influenza. Although such bacterial infections can often be treated by antibiotics, these drugs would be either unavailable or in short supply for much of the global population during a pandemic.
The arrival of a pandemic influenza would trigger a reaction that would change the world overnight. A vaccine would not be available for a number of months after the pandemic started, and there are very limited stockpiles of antiviral drugs. Plus, only a few privileged areas of the world have access to vaccine-production facilities. Foreign trade and travel would be reduced or even ended in an attempt to stop the virus from entering new countries—even though such efforts would probably fail given the infectiousness of influenza and the volume of illegal crossings that occur at most borders. It is likely that transportation would also be significantly curtailed domestically, as smaller communities sought to keep the disease contained. The world relies on the speedy distribution of products such as food and replacement parts for equipment. Global, regional, and national economies would come to an abrupt halt—something that has never happened due to HIV, malaria, or TB despite their dramatic impact on the developing world.
The closest the world has come to this scenario in modern times was the SARS (severe acute respiratory syndrome) crisis of 2003. Over a period of five months, about 8,000 people were infected by a novel human coronavirus. About ten percent of them died. The virus apparently spread to humans when infected animals were sold and slaughtered in unsanitary and crowded markets in China's Guangdong Province. Although the transmission rate of SARS paled in comparison to that of influenza, it demonstrated how quickly such an infectious agent can circle the globe, given the ease and frequency of international travel. Once SARS emerged in rural China, it spread to five countries within 24 hours and to 30 countries on six continents within several months.
The SARS experience teaches a critical lesson about the potential global response to a pandemic influenza. Even with the relatively low number of deaths it caused compared to other infectious diseases, SARS had a powerful negative psychological impact on the populations of many countries. In a recent analysis of the epidemic, the National Academy of Science's Institute of Medicine concluded: "The relatively high case-fatality rate, the identification of super-spreaders, the newness of the disease, the speed of its global spread, and public uncertainty about the ability to control its spread may have contributed to the public's alarm. This alarm, in turn, may have led to the behavior that exacerbated the economic blows to the travel and tourism industries of the countries with the highest number of cases."
SARS provided a taste of the impact a killer influenza pandemic would have on the global economy. Jong-Wha Lee, of Korea University, and Warwick McKibbin, of the Australian National University, estimated the economic impact of the six-month SARS epidemic on the Asia-Pacific region at about $40 billion. In Canada, 438 people were infected and 43 died after an infected person traveled from Hong Kong to Toronto, and the Canadian Tourism Commission estimated that the epidemic cost the nation's economy $419 million. The Ontario health minister estimated that SARS cost the province's health-care system about $763 million, money that was spent, in part, on special SARS clinics and supplies to protect health-care workers. The SARS outbreak also had a substantial impact on the global airline industry. After the disease hit in 2003, flights in the Asia-Pacific area decreased by 45 percent from the year before. During the outbreak, the number of flights between Hong Kong and the United States fell 69 percent. And this impact would pale in comparison to that of a 12- to 36-month worldwide influenza pandemic.
The SARS epidemic also raises questions about how prepared governments are to address a prolonged infectious-disease crisis—particularly governments that are already unstable. Seton Hall University's Yanzhong Huang concluded that the SARS epidemic created the most severe social or political crisis encountered by China's leadership since the 1989 Tiananmen crackdown. China's problems probably resulted less from SARS' public health impact than from the government's failed effort to allay panic by withholding information about the disease from the Chinese people. The effort backfired. During the crisis, Chinese Premier Wen Jiabao pointed out in a cabinet meeting on the epidemic that "the health and security of the people, overall state of reform, development, and stability, and China's national interest and image are at stake." But Huang believes that "a fatal period of hesitation regarding information-sharing and action spawned anxiety, panic, and rumor-mongering across the country and undermined the government's efforts to create a milder image of itself in the international arena."
Widespread infection and economic collapse can destabilize a government; blame for failing to deal effectively with a pandemic can cripple a government. This holds even more for an influenza pandemic. In the event of a pandemic influenza, the level of panic witnessed during the SARS crisis could spiral out of control as illnesses and deaths continued to mount over months and months. Unfortunately, the public is often indifferent to initial warnings about impending infectious-disease crises—as with HIV, for example. Indifference becomes fear only after the catastrophe hits, when it is already too late to implement preventive or control measures.
READY FOR THE WORST
What should the industrialized world be doing to prepare for the next pandemic? The simple answer: far more. So far, the World Health Organization and several countries have finalized or drafted useful but overly general plans. The U.S. Department of Health and Human Services has increased research on influenza-vaccine production and availability. These efforts are commendable, but what is needed is a detailed operational blueprint for how to get a population through one to three years of a pandemic. Such a plan must involve all the key components of society. In the private sector, the plan must coordinate the responses of the medical community, medical suppliers, food providers, and the transportation system. In the government sector, the plan should take into account officials from public health, law enforcement, and emergency management at the international, federal, state, and local levels.
At the same time, it must be acknowledged that such master blueprints may have their drawbacks, too. Berkeley's Aaron Wildavsky persuasively argued that resilience is the real key to crisis management—overly rigid plans can do more harm than good. Still, planning is enormously useful. It gives government officials, private-sector partners, and the community the opportunity to meet, think through potential dilemmas, purchase necessary equipment, and set up organizational structures for a 12- to 36-month response. A blueprint forces leaders to rehearse their response to a crisis, preparing emotionally and intellectually so that when disaster strikes the community can face it.
Influenza-vaccine production deserves special attention. An initiative to provide vaccine for the entire world must be developed, with a well-defined schedule to ensure progress. It is laudable that countries such as the United States and Vietnam are pursuing programs with long-term goals to develop and produce H5N1 vaccine for their respective populations. But if the rest of the world lacks supplies, even the vaccinated will be devastated when the global economy comes to an abrupt halt. Pandemic-influenza preparedness is by nature an international issue. No one can truly be isolated from a pandemic.
The pandemic-related collapse of worldwide trade and its ripple effect throughout industrialized and developing countries would represent the first real test of the resiliency of the modern global delivery system. Given the extent to which modern commerce relies on the precise and readily available international trade of goods and services, a shutdown of the global economic system would dramatically harm the world's ability to meet the surging demand for essential commodities such as food and medicine during a crisis. The business community can no longer afford to play a minor role in planning the response to a pandemic. For the world to have critical goods and services during a pandemic, industry heads must stockpile raw materials for production and preplan distribution and transportation support. Every company's senior managers need to be ready to respond rapidly to changes in the availability, production, distribution, and inventory management of their products. There is no model for how to revive the current global economy were it to be devastated.
To truly be complete, all planning on international, regional, national, and local levels must consider three different scenarios: What if the pandemic begins tonight? What if it starts one year from now? What if the world is so fortunate as to have an entire decade to prepare? All are possible, but none is certain.
STARTING TONIGHT
What would happen today in the office of every nation's leader if several cities in Vietnam suffered from major outbreaks of H5N1 infection, with a five percent mortality rate? First, there would be an immediate effort to try to sort out disparate disease-surveillance data from a variety of government and public health sources to determine which countries might have pandemic-related cases. Then, the decision would likely be made to close most international and even some state or provincial borders—without any predetermined criteria for how or when those borders might be reopened. Border security would be made a priority, especially to protect potential supplies of pandemic-specific vaccines from nearby desperate countries. Military leaders would have to develop strategies to defend the country and also protect against domestic insurgency with armed forces that would likely be compromised by the disease. Even in unaffected countries, fear, panic, and chaos would spread as international media reported the daily advance of the disease around the world.
In short order, the global economy would shut down. The commodities and services countries would need to "survive" the next 12 to 36 months would have to be identified. Currently, most businesses' continuity plans account for only a localized disruption—a single plant closure, for instance—and have not planned for extensive, long-term outages. The private and public sectors would have to develop emergency plans to sustain critical domestic supply chains and manufacturing and agricultural production and distribution. The labor force would be severely affected when it was most needed. Over the course of the year, up to 50 percent of affected populations could become ill; as many as five percent could die. The disease would hit senior management as hard as the rest of the work force. There would be major shortages in all countries of a wide range of commodities, including food, soap, paper, light bulbs, gasoline, parts for repairing military equipment and municipal water pumps, and medicines, including vaccines unrelated to the pandemic. Many industries not critical to survival—electronics, automobile, and clothing, for example—would suffer or even close. Activities that require close human contact—school, seeing movies in theaters, or eating at restaurants—would be avoided, maybe even banned.
Vaccine would have no impact on the course of the virus in the first months and would likely play an extremely limited role worldwide during the following 12 to 18 months of the pandemic. Despite major innovations in the production of most other vaccines, international production of influenza vaccine is based on a fragile and limited system that utilizes technology from the 1950s. Currently, annual production of influenza vaccine is limited to about 300 million trivalent doses—which protect against three different influenza strains in one dose—or less than one billion monovalent doses. To counter a new strain of pandemic influenza that has never circulated throughout the population, each person would likely need two doses for adequate protection. With today's limited production capacity, that means that less than 500 million people—about 14 percent of the world's population—would be vaccinated within a year of the pandemic. In addition, because the structure of the virus changes so rapidly, vaccine development could only start once the pandemic began, as manufacturers would have to obtain the new pandemic strain. It would then be at least another six months before mass production of the vaccine.
Even if the system functions to the best of its ability, influenza vaccine is produced commercially in just nine countries: Australia, Canada, France, Germany, Italy, Japan, the Netherlands, the United Kingdom, and the United States. These countries contain only 12 percent of the world's population. In the event of an influenza pandemic, they would probably nationalize their domestic production facilities, as occurred in 1976, when the United States, anticipating a pandemic of swine influenza (H1N1), refused to share its vaccine.
If a pandemic struck the world today, there would be another possible weapon against influenza: antiviral medicine. When taken daily during the time of exposure to influenza, antivirals have prevented individuals from becoming ill. They have also reduced the severity of illness and subsequent complications when taken within 48 hours of onset. Although there is no data for H5N1, it is assumed antivirals would also prevent H5N1 infection if taken before exposure. There is no evidence, however, that current antiviral influenza drugs would help if the patient developed the kind of cytokine storm that has characterized recent H5N1 infections. But barring this complication, H5N1 should be treatable with Tamiflu (oseltamivir phosphate), which is manufactured by the Roche pharmaceuticals company in a single plant in Switzerland.
In responding to a pandemic, Tamiflu could have a measurable impact in the limited number of countries with sizable stockpiles, but for most of the world it would not be available. Although the company plans on opening another facility in the United States this year, annual production would still cover only a small percentage of the world's population. To date, at least 14 countries have ordered Tamiflu, but the amount of these orders is enough to treat only 40 million people. The orders take considerable time to be processed and delivered—manufacturing can take up to a year—and in an emergency the company's ability to produce more would be limited. As with vaccines, countries would probably nationalize their antiviral supplies during a pandemic. Even if the medicine were available, most countries could not afford to buy it. Critical antibiotics, for treatment of secondary bacterial infections, would also be in short supply during a pandemic. Even now, supplies of eight different anti-infective agents are limited in the United States due to manufacturing problems.
Aside from medication, many countries would not have the ability to meet the surge in the demand for health-care supplies and services that are normally taken for granted. In the United States, for example, there are 105,000 mechanical ventilators, 75,000 to 80,000 of which are in use at any given time for everyday medical care. During a routine influenza season, the number of ventilators being used shoots up to 100,000. In an influenza pandemic, the United States may need as many as several hundred thousand additional ventilators.
A similar situation exists in all developed countries. Virtually every piece of medical equipment or protective gear would be in short supply within days of the recognition of a pandemic. Throughout the crisis, many of these necessities would simply be unavailable for most health-care institutions. Currently, two U.S.-based companies supply most of the respiratory protection masks for health-care workers around the world. Neither company would be able to meet the jump in demand, in part because the component parts for the masks come from multiple suppliers in multiple countries. With travel and transportation restricted, masks may not even be produced at all.
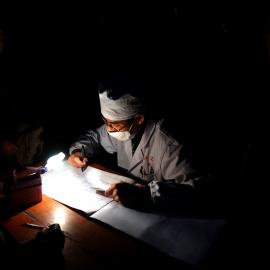
Health-care providers and managed-care organizations are also unprepared for an outbreak of pandemic influenza today. There would be a tremendous demand for skilled health professionals. New "hospitals" in high school gymnasiums and community centers would have to be staffed for one to three years. Health-care workers would probably get sick and die at the same rate as the general public—perhaps at an even higher rate, particularly if they lack access to protective equipment. If they lack such fundamental supplies, it is unclear how many professionals would continue to place themselves in high-risk situations by caring for the infected. Volunteers who are naturally immune as a result of having survived influenza infection would thus have to be found and employed. That means that the medical community's strong resistance to using lay volunteers, which is grounded in both liability concerns and professional hubris, would need to be addressed.
Other unpleasant issues would also need to be tackled. Who would have priority access to the extremely limited antiviral supplies? The public would consider any ad hoc prioritization unfair, creating further dissent and disruption during a pandemic. In addition, there would not even be detailed plans for handling the massive number of dead bodies that would soon outstrip the ability to process them. Clearly, an influenza pandemic that struck today would demand an unprecedented medical and nonmedical response. This requires planning well beyond anything devised thus far by any of the world's countries and organizations.
A YEAR FROM NOW
Even if an H5N1 pandemic is a year away, the world must plan for the same problems with the same fervor. Major campaigns must be initiated to prepare the nonmedical and medical sectors. Pandemic planning must be on the agenda of every school board, manufacturing plant, investment firm, mortuary, state legislature, and food distributor in the United States and beyond. There is an urgent need to reassess the vulnerability of the global economy to ensure that surges in demand can be met. Critical health-care and consumer products and commodities must be stockpiled. Health professionals must learn how to better communicate risk and must be able to both provide the facts and acknowledge the unknowns to a frightened or panicked population.
If there is a year of lead-time before an H5N1 pandemic, vaccine could play a more central role in the global response. Although the world would still have a limited capacity to manufacture influenza vaccine, techniques that could allow scientists to get multiple doses from a current single dose may increase the supply. In addition to further research on this issue, efforts are needed to ensure the availability of syringes and equipment for delivering vaccine. There must also be an international plan for how the vaccine would be allocated. It is far better to struggle with the ethical issues involved in determining such priorities now, in a public forum, rather than to wait until the crisis occurs.
Prevention must also be improved. Priority should be placed on early intervention and risk assessment. And an aggressive and comprehensive research agenda must be launched immediately to study the ecology and biology of the influenza virus and the epidemiologic role of various animal and bird species.
TEN YEARS LATER
If developed countries begin to transform radically the current system of influenza-vaccine production, an influenza pandemic ten years from now could have a much less devastating outcome. The industrialized world must initiate an international project to develop the ability to produce a vaccine for the entire global population within several months of the start of a pandemic. The initiative must be a top priority of the group of seven industrialized nations plus Russia (G-8), because almost nothing could inflict more death and disruption than a pandemic influenza.
The current BioShield law and additional legislation recently submitted to Congress will act to enhance the availability of vaccines in the United States. This aim is laudable, but it does little to address international needs. The ultimate goal must be to develop a new cell-culture vaccine or comparable vaccine technology that works on all influenza subtypes and that can be made available on short notice to all the people of the world.
WHAT COURSE TO TAKE?
The world must form a better understanding of the potential for the emergence of a pandemic influenza strain. A pandemic is coming. It could be caused by H5N1 or by another novel strain. It could happen tonight, next year, or even ten years from now.
The signs are alarming: the number of human and animal H5N1 infections has been increasing; small clusters of cases have been documented, suggesting that the virus may have come close to sustained human-to-human transmission; and H5N1 continues to evolve in the virtual genetic reassortment laboratory provided by the unprecedented number of people, pigs, and poultry in Asia. The population explosion in China and other Asian countries has created an incredible mixing vessel for the virus. Consider this sobering information: the most recent influenza pandemic, of 1968-69, emerged in China, when its population was 790 million; today it is 1.3 billion. In 1968, the number of pigs in China was 5.2 million; today it is 508 million. The number of poultry in China in 1968 was 12.3 million; today it is 13 billion. Changes in other Asian countries are similar. Given these developments, as well as the exponential growth in foreign travel over the past 50 years, an influenza pandemic could be more devastating than ever before.
Can disaster be avoided? The answer is a qualified yes. Although a coming pandemic cannot be avoided, its impact can be considerably lessened. It depends on how the leaders of the world—from the heads of the G-8 to local officials—decide to respond. They must recognize the economic, security, and health threat that the next influenza pandemic poses and invest accordingly. Each leader must realize that even if a country has enough vaccine to protect its citizens, the economic impact of a worldwide pandemic will inflict substantial pain on everyone. The resources required to prepare adequately will be extensive. But they must be considered in light of the cost of failing to invest: a global world economy that remains in a shambles for several years.
This is a critical point in history. Time is running out to prepare for the next pandemic. We must act now with decisiveness and purpose. Someday, after the next pandemic has come and gone, a commission much like the 9/11 Commission will be charged with determining how well government, business, and public health leaders prepared the world for the catastrophe when they had clear warning. What will be the verdict?
You are reading a free article.
Subscribe to Foreign Affairs to get unlimited access.
- Paywall-free reading of new articles and a century of archives
- Unlock access to iOS/Android apps to save editions for offline reading
- Six issues a year in print, online, and audio editions